by Dr. Mahesh Kulkarni
Introduction :-
Approximately 50 lakh joint replacement operations are done each year worldwide. Although most people who undergo this type of surgery are over the age of 50-60, about a quarter are younger than 50. Damage to the knee or hip joint can result from various reasons but the most common cause is Arthritis. Surgery to replace all or part of a damaged knee or hip joint can have a dramatic effect on the lifestyle of someone suffering from severe pain and disability. But it is a major operation which should not be undertaken lightly. Your consultant will advise you about the likely benefits of surgery, but the final decision to go ahead is yours. Before making that decision you should be sure that your expectations about its outcome are realistic and that you understand the surgery. We hope this article will provide enough information to help you make an informed decision.
Tests and Decisions
People suffering from severe pain and disability seek advice of the specialist. Firstly the patient is treated with medication and physiotherapy. When these measures fail to give relief from pain and disability the specialist may suggest you about the joint replacement surgery.
The joint replacement surgeon will examine you, will see your x-rays and eventually will suggest you about the joint replacement surgery. The possible outcomes and risks of the surgery and anesthesia are explained to you. Though the doctor suggests surgery to you, the final decision must be yours, depending on the extent you suffer from pain.
There are some factors which should be taken into account before going for the operation.
- Daily Activity:-
If you are physically very active and relatively young you should consider other options like physiotherapy and medical therapy. So that you can postpone the surgery as much as possible, as more strenuous activity may reduce the life of the implants. - The quality of your Bone and Muscle:-
As metal parts are to be inserted in your bone, your bone should have a good quality, so that they fit into the bones for a fairly longer time. Also the quality of your muscles should be good, so that you can carry out the post-operative physiotherapy programme to build your muscles. - Your General Physical Condition:-
If you are suffering from arthritis in other joints, your daily activities may be restricted despite operation of knee or hip joint - Your medical problems might increase the risk of surgery and anaesthesia.
Knee Replacement

PROSTHESIS OF KNEE JOINT:
The doctor will decide about the best material to be used in your particular case.
This selection will depend upon factors such as –
- Your Age and Normal Level of Activity.
- Degree of Damage.
- Deterioration of the Bones of your Knee Joint.
- Femoral Component: It is the part which fits onto the thigh bone. It is made of highly polished alloy like cobalt, chrome, oxinium.
- Tibial component: This is like a tray. It is also made of metal like Titanium. It comes with a highly cross linked plastic dish like structure together they make the tibial component.
- Patellar Component: It fits on the patella. It is also made of highly cross linked plastic.
All these components are fitted over respective bones with the help of bone cement. - Oxidized Zirconium: Is a tough Zirconium alloy metal substrate which decreases the wear as a result of which life of joint increases.
Systems used during Total Knee Replacement surgery (TKR)
The following systems are helpful to the surgeon while performing surgery, which decreases duration of surgery & increases accuracy.
- Computer Navigation: This system allows surgeon to take help of computer during surgery. This increases accuracy of surgery, which in turn increases the long term success of operation.
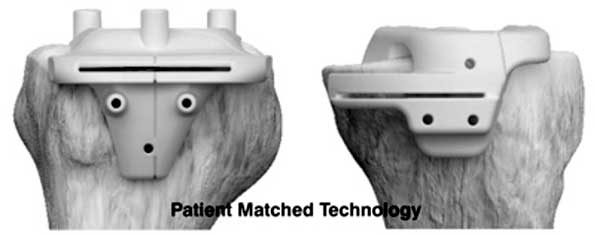
- Patient Matched Technology: In this most modern technology, patients MRI Scan and Xrays are sent to Engineers in the United States.
They prepare specific blocks for individual patients. This helps in making the surgery faster and more accurate. This also helps in increasing the long term results of surgery
Possible Post Operative Complications
These are some common complications associated with each type of surgery & some are specifically related to hip replacement surgery. Most complications are minor but it is important to be aware & to seek medical attention.
- Chest Infection –
Possible following general anaesthesia and particularly in smokers.- Deep breathing is important
- Fever –
It can develop in the first 24-72 Hrs, after surgery. Its cause will have to be investigated and treated accordingly. - Thrombosis & Embolism –
After surgery blood clot (deep vein thrombosis) may occur in one of the deep veins of the body.- We take precautions to prevent this from happening.
- Wearing Anti-Embolism stockings : at least for 6 weeks.
- Course of blood thiner Injections/Tablets.
- Exercises & Early Mobilization after surgery.
- Infection –
It is always a risk when materials are implanted into the body.

- We use special precautions to avoid this
- Operation theatres with laminar flow.
- Operating Staff with disposable suits. (Space Suits)
- Antibiotics in peri operative period.
- Sepsis –
Sepsis may be caused by pus producing organisms. Main cause is contamination of the wound.- You need to take proper medical advice if you have pain, swelling, heat and redness around wound or with leakage of pus and high fever.
- Nerve Damage –
The small nerves supplying the skin over operation site are usually damaged. When an incision is made during surgery it can cause numbness around wound. This does not in any way affect the function following surgery
Before Your Operation
After your decision to go in for a joint replacement you should be aware of the basic things to be done before surgery. Such as –
- Suitable prosthesis for you.
- The cost of your prosthesis.
- Total Hospital stay & cost of hospital stay.
- The Blood, Heart and Chest investigations.
- Get this investigations 2-3 weeks before the date of surgery & get them checked by a physician.
- It is necessary to confirm that there is no active infection in your body.
- If you have mediclaim facility, you should contact hospital’s mediclaim department at least one week before surgery with your policy documents.
- You should show the drugs which you are already taking. Some types of medicines like steroids & blood thinning medicines are to be stopped 5-7 days prior to surgery.
- For admission in hospital take admission letter from your surgeon.
- You may advised to get admitted 1-2 days prior to the surgery. Take all investigations report, previous medical records & drugs with you.
Peri-Operative Protocol
After admission –
After you are admitted in the hospital, a resident/registrar doctor will come to you. He will examine you again & explain you in brief things to be carried out before & after the operation. A physician will come & examine you & will give the fitness for surgery.Anaesthetist Visit –
Anaesthetist will come to you & will examine you from the view of anesthesia. He will explain to you in brief the type of anaesthesia, drugs to be stopped & the drugs to be taken on the day of surgery. You will be asked to stop taking food or drinks at least 6 – 8 hrs. before surgery.Anaesthesia –
Anaesthesia will be spinal & epidural in which the lower part of your body will be anaesthetized. You will be awake during surgery. A thin plastic tube will be inserted into your back through which anaesthetic drug along with pain killers will be induced in your body. Because of this you will feel numbness in your legs. This tube may kept in your back for couple of days for pain relief.Bathing –
You will be asked to have bath on the previous night of surgery & a couple of hours before surgery, to maintain cleanliness of your body & operation site.After your operation –
After surgery you will be kept in the recovery room for couple of hours. After that you will be shifted to your room. You will be asked to keep fasting for 4-6 hrs. after surgery. After that you can start orally with clear liquids first. If there is no vomiting, you can have a light diet on the night of surgery.Drips –
There may be an intravenous drip for next 2 – 3 days for admission of antibiotics, saline & fluids. Once you will start taking food orally, saline & fluids will be discontinued but antibiotics will be continued for the next couple of days.Wound Drains –
There may be one or more small plastic tubes extending out of the side of the wound dressing, draining into a bottle. These tubes enable excess fluid & blood to drain away from the wound. Dressing will be checked & changed as required. Pillow will be given under calf to avoid pressure sores.
Simple Exercises –
You are advised to do some simple exercise before & after operation. You should start them as soon as possible when you are still in recovery room or shifted to your room.
- Deep Breathing – Deep breathing and coughing will help to keep your lungs supplied with oxygen & clear the sputum.
- Leg Execises – Simple leg exercises will help to reduce risk of deep vein thrombosis & can easily be done. Some of them will also help mobilize your hip joint & strengthen your muscles.
- Foot Flexion & extension & circular movements. (fig. 1)

- Lying on your back, press your kness on to the bed with your leg straight. (fig.2)
Pain Relief –
If you have had an epidural anaesthesia, pain killer drug may be infused through it.
After first couple of post operative days, regular pain killers will probably provide sufficient pain relief, likely to be continued for several weeks to enable you to do necessary exercises.
In hospital, if your pain is not being controlled kindly inform a doctor or nurse, as it may be possible to give you stronger pain killers.
Thrombosis Prevention –
Blood clots are most common about 2 days after surgery. Although they can develop any time upto 3 weeks later.
Prevention-
- Daily injection of low dose anti-coagulant or tablet until you are in hospital.
- You will be asked to wear anti-embolism stockings for upto 6 weeks after surgery.
Blood Test –
A sample of your blood will be taken to measure hemoglobin level. If hemoglobin is low –
- You May be started on iron tablets.
- Sometimes blood trans fusions are required.
X-rays –
An x-ray will be taken of your operated joint, either in the recovery room or within 48 hrs. after operation.
Bladder Function –
You will have a urinary catheter that will drain your urine from your urinary bladder. It will kept there for the next 3-4 days until you are able to urinate voluntarily in a bed pan or commode-chair near bedside.
Physiotherapy

- Car Transfera.
- Getting into a car –
- Be sure the passenger seat is pushed all the way back.
- Recline the seat back as far as possible.
- With your walker in front of you, slowly back up to the car seat.
- Sit on the car seat.
- Swing your legs into the car.
- When traveling make frequent stops and get out & walk around.

- Getting out of car –
- Push the seat all the way back.
- Recline the seat all the way back.
- Lift your legs out. Place the walker up in front of you & stand up on the unaffected leg or leg which is having less pain.
- Getting into a car –
- Climbing up stairs:-
- Climbing up stairs-
- Use a hand rail (if available) to climb stairs.
- Lead with your non – operated leg or less painful leg, then operated leg and finally your crutches or cane.
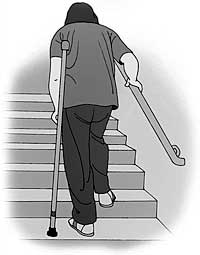
- A family member should stay one step below helping you to climb stairs.
- Going down stairs –
- Use a hand rail (if available) to go down stairs.
- Lead with your crutch or cane, then your operated leg and finally non- operated or less painful leg.
- A family member should stay one step below, helping you to go down stairs.

- Climbing up stairs-
- Chair transfer:-
- Back up to the chair until you feel both legs touching the chair.

- Slide your operated leg out in front of you, place one hand on the armrest.
- Lower your self slowly, keeping your operated leg straight out.
- When getting up, scoot your operated leg out in front of you until you can stand on it comfortably.
- Push up using the armrests, keeping your operated leg out in front of you.
- Back up to the chair until you feel both legs touching the chair.
- Walking –
- A physiotherapist will help you to walk a short distance with walker.

- After couple of days, you may be able to progress to walking with a walker independently.

- A physiotherapist will help you to walk a short distance with walker.
