by Dr. Vinaya Kunjir & Dr. Vaijayanti Lagu – Joshi
Osteoarthritis is one of the most frequently observed arthritis in elderly population, mostly neglected as aging or degenerative arthritis. But with modernization, changing lifestyles and longevity of life, this type of arthritis is becoming of more concern. In the last 3 issues of MAI magazines, we have given information mostly on inflammatory arthritis group like rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis. However, osteoarthritis is much more common than the inflammatory groups, in a population. We will be trying to give information on a few aspects of osteoarthritis in this issue of MAI magazine.
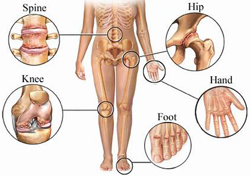
The following image shows the joints most often affected by osteoarthritis :
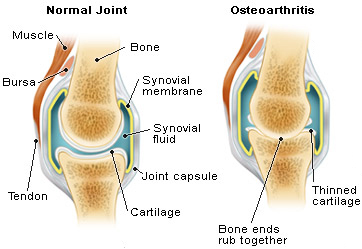
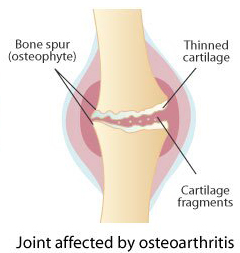
Osteoarthritis is a progressive disease characterized by loss of articular cartilage , along with extensive sclerosis and remodeling of bone adjacent to cartilage and joint margins resulting in formation of osteophytes. This process can be de novo as in primary osteoarthritis or secondary phenomenon as a result of damage due to other disease processes like inflammatory arthritis, or abnormal anatomy of bones or joints as in congenital disorders, or trauma.
Osteoarthritis can be localized to one joint region, eg. nodules over distal phalange joint of hands. It can be generalized involving two or more joint areas as shown in Image 1. The commonest joints involved are the knees, spine (cervical, lumbar), hip, the weight bearing joints.
Why does Osteoarthritis occur ?
Aging, obesity, lack of exercises, heredity, injuries / trauma, abnormal joint mechanics, certain occupations, stress and strain hasten the process of wear and tear. Pain in joints on activity, occasionally swelling, creaky noise (crepitus) during movements, restriction of movements and disability are common manifestations.
The process is obviously progressive, but is there anything that can be done about it ? Yes. Although we cannot stop the process completely, we can retard the rate of progression by a variety of measures.
There are always many ways to reach the goal.
- Medications like glucosamine, chondroitin sulphate are promising in very early or extremely advanced osteoarthritis. Analgesics, painkillers, intra-articular hyaluronic acid injections are all for symptomatic relief.
- Complementary pathies like ayurved, homeopathy do have some potential drugs which need to be evaluated in clinical trials. Inspite of medical / surgical therapies, one needs to follow some non pharmacological means throughout therapy schedule.
- The patient needs to control body weight in a proper range of dietary restrictions and exercise programme.
- The habits of tobacco / smoking are not at all advisable.
- The everyday standing, walking, sitting and working postures need to be very well looked after.
- Exercise schedule should be a part of the daily routine. Health cycling, daily walking on flat surface, following some relaxation techniques like yoga, pranayam are all complementary to build up muscle power and good mobility of joints. However, for severely advanced osteoarthritis causing extreme disability need corrective surgery or replacement.
After all, prevention is better than cure. We cannot stop aging, but yes, we can stop premature “aging”and painful / disabling aging. The therapy approaches are individualized as per treating doctor’s and patient’s wish.
Cartilage transplants, bioprosthesis, stemcell implants are the future of osteoarthritis. This “degeneration”is no “dead-end”, but can be the beginning of a new era.
Why Does My Knee Hurt
by Dr. Arvind Chopra
Why Does My Knee Hurt ?
A knee is a hinge joint and it moves like opening of a window or a door. Storng thigh (femur) and calf (tibia) bones meet in the joint. To avoid bone to bone contact the free end of bones in the joint is covered with cartilage. Another thick layer of cartilage, shaped like “C: called meniscus, lies between the cartilage covered free bone ends. Cartilage, unlike bone, is not visible on a X-Ray. But cartilage is firm and resilient ( can absorb fluid like a sponge when in a resting position, and the same fluid is squeezed out when it is pressed in standing / running position ) in structure that absorbs all kinds of “shock”- ranging from standing for prolonged periods to dancing and jumping. There is an oily fluid in the knee joint meant for lubrication & to provide nutrition to cartilage. Few ligaments inside the depth of knee joint called “cruciate ligament”hold the free ends of femur & tibia together. The joint along with its bone, Cartilage, ligament and fluid is enclosed by a fibrous capsule, much like the outside of a dry coconut. Inside this capsule is line by a fine delicate membrane called synovial membrane that extends onto the bone ends in the joint but not over cartilage. Synovial membrane is rich in blood supply and is composed of different types of cells, several of which are competent to fight bacteria, viruses and any foreign particles. The synovial membrane can be considered as another part of the body immune (defence) system. Several muscles (e.g. thigh muscles) are inserted (through tendons) into the bone close to the knee joint and provide support and movement Several ligaments bind the end of bones outside the capsule to strengthen the joint structure. A circular piece of bone called knee cap or patella lies in the front part of the knee joint, and is kept in position by surrounding muscles fibres and ligaments. Finally the knee joint has its own blood supply and nerve. If you closely examine your knee, you will realise how easy it is feel the bony parts including knee cap. On the sides, there is hardly any coverying y nuscles or fat. All this makes the joint prone to injuries. There are several reasons for the knee to hurt and become painful. In fact, everyone experiences a painful knee some time or the other. It is important to know that different causes predominate at different ages. Let us go through some broad classification of causes
Injuries
Falls & accidents often damage the knee. The exact nature of injury is important to recognize before diagnosing the likely structural damage. Sometimes, the impact of injury is deep inside the painful knee and superficial clinical examination and X-Ray may not reveal any abnormality. A common early consequence of a significant knee injury is a painful swelling of knee due to fluid / blood collection inside. Small cartilage tears, especially to meniscus, can be caused by injuries sustained in sports and athletes. Injuries sometimes even trivial, are the commonest causes of knee pain in the young.
Degeneration
Commonly described as “wear & tear”. The primary damage is in the cartilage, which may progress on abnormal or excess knee loading in certain unaccustomed activities, be it jogging or even long walks. Sudden spurt of physical activity like aerobics or treadmill exercise in an untrained person can worsen cartilage degeneration and cause pain. Knee injuries if not treated properly can lead to cartilage degeneration & knee pain. Remember that age itself can cause slow progressive cartilage degeneration but clinically by itself this causes knee pain well past 65 years age. Irrespective of the precise cause, cartilage degeneration with poor healing leads to several mechanical abnormalities in the knee structure and function. Each can cause different type & site of knee pain. The disease that is caused by such primary cartilage damage is called osteoarthritis. Often, the patient develops bow legs called varus deformity. So osteoarthritis per se may be a cause of serious knee pain in late sixties or early seventies unless complicated by injuries or excess body weight in earlier years of life.
Inflammation
These disorders are characterized by painful swellings that are red and warm. They can be extremely painful confining the patient to chair and bed in a short period of time.
Non – Infective – Inflammatory knee arthritis is commonly due to rheumatoid arthritis, rheumatic fever arthritis, reactive arthritis, juvenile inflammatory arthritis, Psoriatic arthritis, etc. These disorders are non – infective which means that they are not directly caused by bacteria, viruses etc. There is no pus in the joint. These disorders may have a genetic background and run in families. They are often referred to as auto-immune disorders that is the body damages its own organ due to altered or abnormal immune system. Some of the cells meant to fight germs begin to attack and damage their own friends – in this case a structure like the joint. The primary seat of damage is the “synovial lining”that sometimes begins to grow like the roots of a tree.
This damages several structures in the joint – bone, cartilage, ligaments, etc. Eventually the joint may become painful & deformed, so unable to bear body weight or more properly. These disorders often involve multiple joints – small & large.
Infective knee arthritis due to bacteria and viruses is uncommon. It causes an acute or a chronic painful knee in people who are otherwise weakened due to other diseases like cancer, diabetes, severe blood infections etc. The synovial fluid becomes pus like and the patient often runs high fever and is very sick. Some infections cause slowly progressive chronic arthritis usually in a single joint – a classical example is tuberculosis of the knee or hip joint which causes swollen joint that is relatively less painful with a limp. Infections usually affect one or few joints.
Other Causes
Some people are born with a somewhat altered knee structure due to bone or cartridge abnormality. The alignment of upper & lower leg at knee may be abnormal. Person may have severe bow legs (varus) or legs shaped like an inverted V (valgus) – both of which may mechanically stress knee during prolonged strenuous job. Sometimes excess mobility at knee joint (or knee cap) can lead to a relatively mild form of knee arthritis in postures of prolonged knee loading, e.g. standing, jogging, walking. Also hyper mobile (excess movements) knees are prone to injuries. Excess body weight per se can lead to early degeneration of cartilage & knee pain. Obesity is a key risk factor in causing / aggravating knee osteoarthritis.
Uncommonly, certain metabolic diseases like gout can cause acute severe painful knee. Gout is due to deposition of uric acid crystals in the joint as a result of high blood uric acid levels. Gout is predominantly a disease of men and usually attacks big toe in feet.
So, why does the knee hurt ?
There can be so many causes as described above. But don’t worry. The usual causes are mild, self limiting or requiring simple remedial measures. Here is a list of common & less serious causes (at least in the beginning) that you must check prior to considering serious diseases:-
- Overweight – If you ignore this, one-day it will become serious.
- Bad posture and position during work& relaxation – keep your feet nicely on even plain ground during prolonged body weight bearing activities. This holds true for preventing ankle, hip & back pains also. Avoid repetitive bending of knees or kicking like starting a scooter etc.
- Bad shoes / foot wear – check your shoe / foot wear for worn out parts. Also ensure that your heel does not sink into shoe heel while walking or standing. While walking, the entire foot should comfortably fit into the size of the shoe / foot wear.
- Improper way of playing certain games (e.g. football) or taking part in athletic activities.
Finally, take care of knees. They have to last a lifetime. Don’t misuse or abuse them. Be kind to your knees.
Arthritis & my Grandmother
by Dr. Arvind Chopra
“Oh Dear Lord! I don’t want to live (with pain and Arthritis)”, moaned my pious grandmother, holding her painful knee with arthritic hands. I tried telling her that she need not live with pain (and arthritis). After all, I am a doctor (and that too a rheumatologist which makes no sense to her “). “Yes! And you ar the greatest”(which she loves to proudly claim to the World but will not tell you how much she hates my medicine). She smiled and simply said, “And you want me to live on medicines”. I tried to gently remind her that the religious scripts are full of instances when the good old Lord called for a physician.’Arthritis’must have been one of his many worldly problems. She smiled and grudgingly agreed for a’small’tablet and one injection. I quietly broke another tablet into small pieces and mixed it with her food. I could not bear to see her in pain and not be able to walk to her prayers. Why can’t we consider medicine as’prasad’/ gift from God? After all, it does relieve pain and we can walk and pray. But then my grandmother was smart enough to tell me that’prasad’, unless eaten in plenty (to cause stomach upset), has no side effects. “That’s fine but can “prasad “relieve pain and arthritis? “Yes! If you have faith in God”. I cannot think of anyone who has more faith in God than my suffering grandmother. But i dare not say that to my grandmother. It would be so Un-Godly (and consumer unfriendly). And i have often heard her say that pain and suffering are gifts from God. My father shared the same sentiment and furhter believed that only the brave and fortunate can share God’s divine work by tolerating pain.My late father suffered from a painful hip arthritis in old age for over three decades with very little complaint. But thank God that he had no problem taking pain killers (sometimes round the clock) as far he remained active and mobile. He took all the necessary precautions and never suffered from any side-effects. I could never really make a clear distinction between ‘pain’ and ‘arthritis’ to my aging dear ones. According to them, it made no difference as they were two sides of the same coin. With passing years, I have now begun to see the practical wisdom of that paradigm. But the gist of the story is that mangaing pain and arthritis in the elderly can be very challenging and frustrating task. And though, I have had a hard time ( not very successful but very dearand memorable) treating arthritis of my grandmother and father, let me share my views on the subject (of arthritis in the elderly) with you dear readers.
My father and grandmother are no different. I have often heard similar desires and sentiments expressed by patients suffering from prolonged painful arthritis. The plea is usually more serious with the elderly who often live with a compromised life. The elderly usually crave (or dream) for self reliance, independence (in life) and peace of mind. “I know happiness is elusive but I should be able to confidently look after myself with dignity and enjoy my walk.” Several charms of the younger days are no longer valid or desirable. But mobility and functional ability are of prime concern. Though not fatal (unlike heart ailments), arthritis is the biggest threat to this invaluable asset of old age.
Age, aging and death are absolute truths. For a large part of life, we do not think too much about them. But sometimes premature events compel us to acknowledge these truths and their consequences on health (and actually life per se). A sudden illness like arthritis or an early age heart attack can be an unpleasant reminder. We ought to prepare ourselves for the change. Often we do not heed warnings of failing health in our middle years and mistakenly attribute them to old age. And worse still, we begin to call old age a disease. Aging begins soon after birth and along with old age is as much a physiological phenomenon as is pregnancy or menopause. The distinction between aging, old age and poor health is often clouded by our perceptions and how people view us. It is usual to expect some aches and pains in old age. But pain and disability which often characterize arthritis can catch the most careful amongst us by total surprise. The surprise may be less in the case of elderly person. Because we generally believe that old age is synonymous with pain, disability and arthritis, Sadly, nothing could be further from the truth. Old age like a beautiful sunset or vintage wine that has its own glow, warmth and fulfillment. And arthritis is dull, restless and frustrating. Arthritis can strike at any age. And it behaves somewhat differently with different age groups. But in the elderly, it can easily get masked by the age. The elderly may not bother about early aches and pains. A slowly progressive slow gait may be due to a painful knee but the elderly conveniently attributes it to old age. Bearing pain and physical ailments, at least in our culture, is considered a sign of spiritually healthy and strong old age. Self-denial is often marked in the elderly. Even when the ailment (pain) has progressed to an intolerable stage, and begun to seriously threaten the already compromised quality of life, the elderly will quietly wait for somebody in the family to notice the suffering and raise an alarm. By the time the ailment is actually recognized by the doctor a lot of valuable time has gone waste.
Unlike several diseases, such as diabetes and cancer, pain and arthritis are difficult to hide. All can see it. This is more of a nuisance because good advice is seldom available. And even when provided, it often gets buried into the rest of junk advise by the rest of well meaning friends. The consolation is “Oh ! It is free. What’s the harm in trying it ?” To my mind, this trend is most damaging. And in the case of the elderly, even more so because time is limited and nothing threatens and cripples quality of life (and mobility) more than pain and arthritis.
Also, several elderly believe that nothing much can be done to alleviate pain and arthritis. There is a tremendous dislike for medicine and doctors. I have often heard the elderly complain “What is the point in living if medicines are required (to sustain life) ?” and to make matters worse, there is a tremendous phobia for medicines because of side effects. “‘I’d rather suffer (pain) than have my kidneys and liver fail.” Despite being convinced about the likely benefits (much more than the side-effects), the elderly will themselves reduce the dose to half. Also, after experiencing the benefit, the medicine will be stopped abruptly. People wrongly believe that if medicines (especially pain killers) are taken for prolonged periods their benefit reduces and a dependence develops. Nobody likes to spend money on disease and drugs, and it is probably worst in the case of the elderly. With no source of income other than the savings of the past and modest pension, the expenditure on sickness is viewed as wastage. Elderly (and many of us) are often stingy about spending on life style and health. Sometimes, even the diet is unhealthy and unbalanced. You often see elderly becoming an epitome of simple living and high thinking (only towards the near and dear ones). The self ceases to matter for leisure and pleasure. But they will drive themselves crazy on issues connected with inheritance for the posterity. And there are several more misconceptions, obsessions, myths and unfounded fears that plague the elderly. They all add to make an otherwise healthy and cheerful old age a miserable burden. Worse still, the misery gets multiplied several times if pain and arthritis invade the old age. Medical management of the elderly is a great challenge. But the job is made even more difficult by that extra baggage (some visible and some invisible) carried by the elderly into the medical care arena. And then, even before a doctor takes a step towards healing, the elderly resigns to the inevitable fate and says “God, I can no longer bear this suffering (pain). Please free me from this useless (painful) life.” Actually, in their mind, doctors and medicines are part of the painful process. I have briefly touched upon some of the psychosocial aspects of old age that interfere with the diagnosis and management of old age arthritis, more so if the arthritis is rheumatoid (RA); late onset of RA is sometimes called LORA. Let me now review some specific aspects of rheumatology care for the elderly.
Diagnosis : Earlier the better. If pain persists (and too in a joint) or requires more than the usual pain killer (e. g. paracetamol / crocin) you ought to consult your doctor. Ill defined body aches and pains, early morning stiffness, undue fatigue, loss of body weight, and unexplained continuous fever can sometimes be the initial features of rheumatoid arthritis (RA) and other forms of inflammatory arthritis. RA is generally a progressive painful swollen multiple joint affection that can affect other body systems and lead to joint deformity. However, the commonest joint affection in the elderly is degenerative arthritis (the wear and tear primary cartilage disorder), also called osteoarthritis (OA), and causes symptoms in the knees and spine (commonly called spondylitis of back and / or neck). Elderly men and women can uncommonly suffer from severe painful arthritis, usually affecting the big toe, due to raised serum uric acid. This is called gout. Uncommonly, gout can become chronic and affect multiple joints. Raised serum uric acid can also be associated with kidney stones. Elderly people commonly suffer from soft tissue aches and pains in different regions of the body (back, neck, shoulder, etc) that can be due to different causes – falls & injuries, OA, bad posture, calcium – vitamin D deficiency, undue mental stress, etc. Acute painful limitation of movements in the shoulder due to ‘frozen shoulder’ is a common problem. Osteoporosis, a disorder of weak bones due to loss of bone substance (including calcium), is commonly seen in the elderly. Osteoporosis is often associated with easy fractures, crooked spine and aches and pains (often in the back). There are several other forms of arthritis that can uncommonly affect the elderly.
Remember to tell the doctor about all other ailments that you suffer from and the medicines that you are taking. In fact, keep all the doctors involved with your care informed about the new ailment. No harm in telling the cardiologist that you have been recently diagnosed to suffer from osteoarthritis of the knees and that medicines have been prescribed. Encourage your doctors to talk with each other (not an easy job !) on your case or at least write a brief note that all can read. A doctor must remember to examine the neurological system in detail as neurological disorders (e.g. Parkinsonism) can interfere both in the diagnosis and management or worse still can coexist with a bad arthritis. A clinical impression is fine and both the doctor and the elderly patient may feel that nothing more is required. But some investigations must be done to strengthen the diagnosis. Also, it is essential to assess the general health (e.g, check blood for hemoglobin, blood sugar, blood urea, etc.) when beginning long term anti-arthritic medications.
General Approach to health and Arthritis : Specific therapy ought to be tailor made to suit the individual needs. However, there are some general guidelines for elderly patients consuming arthritis medicines and pain killers in particular, In fact, much of the advice below would be relevant to several other disease situations. The basic physiology of aging with special reference to systems of digestion, metabolism, circulation and hepatic, renal (liver and kidney) excretion must be kept in mind when choosing medicines and their doses. Elderly often have multiple diseases requiring several drugs. And drugs can interact within us – whether it be in the gut (to reduce their absorption), blood stream (to raise or reduce their active fractions) or liver (to interfere with each other’s metabolism). It is too important that the frequency and timings of drugs be well understood, especially with respect to meals. Elderly often have to consume several drugs for several ailments. Elderly are often poor eaters, and doctors must go into details of their eating habits and meal timings.
There are no dietary restrictions for the majority of elderly patients suffering from arthritis. As a general rule, it would be a healthy practice for the elderly to eat some what less rather than overfill the stomach. Overall, the diet should be well balanced in proteins, fats and carbohydrates. Meals should be wholesome, nutritious, pleasing but light. Too much frying and spices should be avoided. It is somewhat easier to ensure freshness and cleanliness for fruits and vegetables. Vegetarian food is easier to cook and digest. Fish is good for the joints and heart. The elderly must be encouraged to eat seasonal fruits (good source for fiber) daily. 300 – 400 ml of good quality milk, probably best in the morning, is advisable. In case of gout (arthritis), proteins (mostly from non-vegetarian diet) need to be curtailed.
Overweight and obesity are going to worsen the suffering (and pain) of arthritis. In this case, the only way to reduce body weight is by an intelligent reduction in the total quantity (calories) of food. Exercise, though essential for general well being, is unlikely to help an elderly patient reduce body weight. Reduce carbohydrates (e.g. bakery products, rice, potatoes, etc.) and fats (mostly from non-vegetarian diets and butter products). A glass of milk (with little cereal / cornflakes) for breakfast, salads and fruits for lunch, and a light enjoyable dinner (just enough to fill the appetite) may suffice for regular intake of medicines and yet ensure slow reduction in body weight. 1 – 2 cups of light tea / coffee, with very little sugar, may be allowed in a day. One boiled egg daily, along with its delicious yellow interior, is not going to worsen your health (or cholesterol), but can provide good proteins and adequate fats. One glass of milk daily is not going to increase your body weight but ensures minimal daily requirements of several essential nutrients including proteins and calcium.
One must drink at least 2 – 3 liters of water, well spaced over 24 hours. Water not only ensures a health kidney-flush system but also helps in healthy bowels and safe drug clearance (from the body). Unfortunately, the elderly (and women in particular) often suffer from poor urinary control and a miserable sleep interrupted by frequent desire to empty the bladder as part of the aging process. Thus, it would be prudent to ensure sufficient water intake during the wakeful day hours and consume it less beyond late evening or early night. But, in case of pain-killers and other anti-arthritis medicine, sufficient water intake is a must. There are other medicines to help improve the bladder control. Sleep is often a serious problem and this could be worse even in case of an otherwise healthy elderly person. 5 – 6 hours of uninterrupted sleep would be refreshing and desirable. If all else (including meditation, Yoga, counseling to reduce worries and stress, etc.) fails, one should not hesitate to ask for sleep medication. Many natural products, including herbal, are in the market to help in sleep and are worth trying. But there are several safe medicine options available today to provide good sleep. A mild tranquilizer may suffice. Don’t be afraid of dependence and addiction as far as you allow yourself to be monitored by a caring and intelligent doctor. Come what may, a good night’s sleep is essential for your old aching creaky joints.
Exercise is essential. But the difficult part is how much and what form ? In case of serious arthritis, the doctor keeping in mind the individual health and disability should prescribe exercise. For most of the mild moderate situations, a daily regimen could consist of a walk and moving all joints (10 – 15 times) systematically though a full range of motion; including moving the neck and back. The speed and length of walk will be determined by your overall health and state of arthritis. 2 – 3 kms of brisk walk can be managed by elderly well into their seventies. The difficult challenge is in case of a bad arthritis. Prolonged loading of moderately severe arthritic knees by standing or walking is likely to make knees worse in time (and take you to the doorstep of an orthopedic surgeon for joint replacement). The latter would hold true for hips and ankles. Swollen joints will become worse with exercise and only need to be moved gently through their range of motion either actively or passively. Care of spine, including back and neck, through proper posture care, both in work and relaxation is essential. Swimming has several benefits for a patient whose arthritis is well controlled with medicines and need to get stronger and better. However certain amount of weight bearing activity (e.g. walking) would be required to prevent and manage osteoporosis. There are several assist devices or simple changes in life style, which can be of great help. A raised toilet seat or a suitable commode will go a long way to heal knee and hip arthritis. Upright chairs with back support (use a small pillow to support back while sitting or traveling) should be used to eat a meal or watch TV. Avoid sofa and low-level sitting. Shoe wear should be proper. No part of the foot should stick out of a chappal or sandal when walking, The elderly are often reluctant to use a walking stick (? symbol of old age) which is an essential aid in case of bad knees, hips and spine.
Home environment should be safe, secure and conducive to living for the elderly. With age, they are prone to dizzy spells, confusion, depression and falls. The family and home environment should be protective. Family support is vital and critical to the well being of the elderly family members. Several problems, including those of health and ailments, become worse when the elderly are compelled to live alone and in isolation. Sometimes, old age homes may be a better choice.
Drugs : Only salient features can be presented in this overview and the readers are advised to discuss their medicines in sufficient detail with their doctor. Often somebody in the family takes the responsibility of administering medicine to the elderly patient. In this case, the caretaker should be familiar with the medicines, their names and dosages. A small mistake can lead to an emergency. Doctors have to exercise special care while writing prescriptions for the elderly – the dose is often reduced. The elderly are sometimes very sensitive to pain-killers and sedatives. It is best to time anti-arthritis medicines along with meals and in fact pain-killers can be taken while eating food (in between a meal). As cautioned above, consume plenty of water. Some elderly patients may feel sleepy after taking oral paracetamol which otherwise is a good painkiller and reduces fever. Oral paracetamol (650 mg) when taken 1 – 3 times daily is an effective and safe pain killer as compared to other drugs (e.g. Brufen, Voveran, etc,) However, if joints are painful and swollen, then an anti-inflammatory painkiller (e.g. Brufen, Voveran) will be required and paracetamol alone may not be enough. Low dose Aspirin is often used to maintain blood fluidity and prevent blood clots so as to avoid heart attack and stroke. If Aspirin is used in higher dose to treat pain or fever this good effect on blood is lost. Thus, elderly people should not use adult dose Aspirin for arthritis. A normal adult dose of a sedative may over sedate the elderly and slow down mental and physical functions. Protection of the stomach is essential when prescribing painkillers and anti-inflammatory drugs for prolonged periods. Enough nutrients and vitamins should be ensured through proper diet and supplement vitamins. Certain blood checks should be done at regular intervals in case of prolonged anti-arthritic medicines. Pain killers can lead to small blood losses in stools through microscopic ulcers in the gut which eventually may cause anemia requiring iron and other supplements – check blood hemoglobin at regular intervals. In case, more potent disease modifying drugs (e.g. methotrexate, sulfasalazine, leflunomide, etc.) are being taken, it is mandatory to check liver and kidney functions, blood hemoglobin and total cell counts at regular intervals. When beginning steroids for severe inflammatory arthritis, great care should be taken to check blood pressure, blood sugar and exclude any infections. Steroids should only be begun when necessary and that too in most appropriate doses for strictly regulated time period. On prolonged steroids, patients need regular monitoring and calcium-vitamin D supplements (to ensure bone health / prevent osteoporosis). Several newer therapeutic options (e.g. anti-TNF therapy for rheumatoid arthritis, parathormone for osteoporosis, etc.) are now available for better efficacy and safety. These newer drugs are being used for the elderly patients also but being expensive their use is still limited in our set up.
Conclusion : Elderly patients need tender love and care perhaps more than the usual adults. Give them human warmth and touch. They should be made to feel ‘needed’ and ‘useful’. With advancing years, the elderly often begin to behave like children. And doctors, nurses and other care providers should remember this when treating them.
At any age, the ailment of an elderly patient demands patient listening and benevolent patience, whether it is from a near relative or a doctor. The majority of my elderly patients love humor and lighthearted philosophy to treat them. Above all, remember that they have seen and experienced the World. Their patience should not be misunderstood as ignorance. Most of the time, it is part of their kindness (not to hurt the doctor with questions and corrections). Actually, they expect much less than what a doctor may think. Give them freedom from pain and freedom to move. Treat them with knowledge, practical experience and tact. And, discuss with them the treatment options before giving them that piece of pa per (write neatly) with to “follow” and “improve life.”
But the difficult and irritating question is “Who is elderly ?” Where is the dividing line ? The looks are often deceptive. The heart remains young (and everyone hopes for it). The brain is sharp (look at some of our ministers !) When I was 30, 60 appeared distant. Now, I am in my 50s and I would like to remain young till I am 70. May be we need to have a bridge for the young elderly. People are living longer and likely to actively contribute well into their 70s. Therefore, a challenge has emerged for the medical fraternity. How are we going to keep our aging community fit ? It is in this respect that the bone and joint health assumes great significance. And, these are times of “The Bone and Joint Decade 2001 – 2010.” The focus is on “quality of life” and “empowering patients.”
But before I sign off, let me add an advice for the young and the aging young and not so old yet. You ought to begin taking care of your bones and joints right in your school days, and continue with the right habits and life style. Only then can you hope to enjoy a healthy and active old age.
Osteoporosis
by Dr. Lata Bichile
A. Deficiency of Vit D/ Calcium/ Oestrogen/ Androgens.
B. Smoking / Alcohol.
C. Inadequate exposure to sunlight.
D. Genetic factors.
E. Immobilisation.
F. Chronic use of certain drugs, steroids.
A. Management of fractures.
B. Suplementation of Vit D / Calcium.
C. Pharmacologic therapy, Estrogen,Bisphosphonates.
A. Balanced diet with calcium / Vit D supplement.
B. Exposure to sunlight.
C. Avoidance of smoking.
D. Regular exercises.
Injury Prevention In The Elderly
by Dr. Satish Kutty
Osteoporosis & Osteomalacia affect nearly everybody in later years of life causing significant
wearing of bones that form a part of the locomotor system of the body.
Osteoporosis also known as brittle bone disease is characterised by poor or deficient formation of bone while
osteomalacia relates to defeciency in its mineralisation.
Injury prevention in elderly consist of following measures :
Injury prevention at home
Ideally the elderly should live in dwellings which are on a single level. Falling off stairs form an important
mechanism & could be avoided by selecting such an arrangement within a home. Rooms should be spacious & well lit with a limited amount of furniture that is absolutely necessary. There should be no barriers between doors & corridors and indeed walking areas should have bannisters for support. Flooring should be of a non slippery type & often times uniform carpeting of the whole dwelling is desirable.
Washrooms should have wet & dry zones with support, particularly applied to walls in the wet area.
Showering or bathing in the wet area should be carried out in a seated posture on a stool or chair fixed to the bath
floor. Bath or shower mat could also aid in providing a nonslippery surface.
The dry area of the washroom should be kept clean and spillproof by wiping the floor, immediately after its use.
A walking aid such as walking stick is usually of a great benefit and one should consider using it as & if deemed
necessary. The aid should have a rubber base & could be of a tripod variety.
Injury prevention while outdoors –
It is best to wear nonslippery & comfortable footwear while going outdoors.
Taking a walking aid, such as stick, usually is a safe practice and one should always try to walk facing the
oncoming traffic, i.e. the right hand side of the road.
It is important to avoid uneven surfaces and paths or roads that have potholes or ditches.
These are some of the measures which could help in the prevention of injuries in the elderly.
