by Dr. Vinaya Kunjir & Dr. Anuradha Venugopalan
Is laboratory testing essential for Rheumatoid Arthritis and other Rheumatic diseases?
The basis of the practice of rheumatology is clinical diagnosis. The history and physical examination of the
patient presenting with symptoms of rheumatic disease are usually diagnostic. However, laboratory testing becomes
extremely essential not only because it provides supportive evidence, but also because the information received from the laboratory tests helps to monitor disease activity.
When does a doctor advise on laboratory tests?
Laboratory tests may either be:
1. Diagnostic tests or
2. Evaluative tests.
Diagnostic tests are those that differentiate individuals who have the disease from those who do not have the disease. These tests are usually concerned only with the current status of the individual being tested.
Evaluative tests are concerned with measuring changes in clinical status or disease activity. The goal of evaluative
testing is to compare the current status of a patient with his status at a previous point of time to determine if
improvement or worsening has occurred. Some laboratory measures may be useful as both diagnostic and evaluative tests. However, some tests that are useful diagnostic tests may not be good evaluative measures.
What are the routine lab test that a patient with rheumatic complaints needs to undergo?
The first time a patient visits the rheumatologist, one needs to have a baseline value of a total body profile along
with the essential diagnostic tests and also some tests to indicate the disease status of the individual. On subsequent
visits, it is essential for every patient on treatment to undergo a minimum number of tests which may indicate either improvement or deterioration of the condition of the patient or for observing any toxicity/adverse effects of the medication.
These include :
1. Haemogram/Complete blood count –
This test includes
Haemoglobin (HB)– It ndicates whether the patient is anemic, the nutritional status and also gives an idea of the disease activity.
Total leucocyte (white cell) count– It is an important test for patients who are on steroids. It is also helpful in
differentiating patients with diseases like SLE, Sjögren’s syndrome, MCTD and Felty’s syndrome, in whom the count
is low from those with Inflammatory Rheumatic Disorders, Systemic Vasculitis and Juvenile Arthritis in whom a high
count is observed.
Differential leukocyte (white cell) count– This test gives and indication of a co-existing infection, vitamin
deficiency, splenomegaly etc.
2. Platelet Count – Platelet count is a measure of disease severity and also a measure of disease activity. This test is very essential and needs to be done every 2-3 months.
3. Erythrocyte Sedementaion Rate – The ESR test is a useful, simple and less expensive test which indicates disease severity. It is also useful for serial measurements when monitoring patients who lack clear clinical markers or who are taking anti-inflammatory or slow-acting antirheumatic drugs. The ESR test is believed to correlate with the severity of inflammatory disease, but some patients with active rheumatic diseases may have a normal ESR level. However, the ESR can also be elevated by conditions unrelated to rheumatic disease, such as aging, anemia, infection, pregnancy, trauma, malignancy
and stress. It is usually higher in women than in men.
4. Rheumatoid Factor(RF) – This is a test used to confirm the diagnosis of Rheumatoid arthritis. However, a negative test does not rule out the diagnosis of Rheumatoid arthritis. Rheumatoid Factor is positive in 75-80% of patients suffering from RA. If RF test is positive, it is essential to quantitate the value further in order to know how strongly positive the test is from the normal range in the given population. An RF value of less than 20 IU/ml is considered normal. In our setting, a value of more than 40 IU/ml is taken as significant. RA patients who are RF negative may sometimes show a
positive RF test a few years after the onset of disease. Similarly, often due to therapy, the RF may become
absent.
5. C-reactive protein(CRP) – The CRP test, just like the ESR, is another marker for disease activity and is an ideal test for following responses to anti-inflammatory treatment. It is not as simple and inexpensive as ESR; it takes a day to perform and requires assay equipment. As with ESR, CRP level/titer can be elevated by pregnancy, trauma and stress, but it does not vary with the patient’s age or sex.
6. Antinuclear Antibody (ANA) Test – This test is a special test done to confirm diagnosis of some rheumatic diseases like SLE, MCTD, Scleroderma etc. 95% patients with SLE test positive for ANA. The ANA titer provides more specific information to the clinician.
7. Anti-DNA Antibody – This test is very useful because a high titer is diagnostic of SLE. The anti-DNA test is also useful therapeutically because it reveals active disease that is not necessarily symptomatic.
8. Serum Uric Acid – This test is usually performed in order to diagnose gout. However, high uric acid levels do not necessarily confirm the diagnosis of gout. High values of serum uric acid are usually associated with an increased risk for the development of gout. Also, it is important to realize that a normal serum urate level does not exclude the diagnosis of
gout. Often a second determination after the acute attack has subsided will show an elevated level.
9. Blood Sugar Level – It is always advisable to get a blood sugar level test done, not only for patients with rheumatic complaints and are of age above 40 years, but also for those patients suffering from some of the other rheumatic diseases and who are on long-term steroids.
10. Liver Function Tests – A mild degree of abnormality in liver function is observed in patients with diseases like SLE. Liver function tests are essential for patients with rheumatic diseases to monitor disease activity and drug toxicity.
11. Kidney Function Tests (Blood urea nitrogen, serum creatinine) – The baseline levels of serum creatinine and blood urea must be known before beginning the treatment with a long term drug. Kidney function tests are also performed as part
of laboratory investigations for collagen vascular disorders e.g. SLE.
Conclusion
Every patient must remember that laboratory data must be interpreted in the light of clinical findings by the specialist, keeping in mind situations when false positives or false negatives may occur. Laboratory tests are mandatory to monitor the disease activity and safeguard against drug toxicity in patients on long-term therapy.
Use of X-rays, C.T. Scan & MRI for diagnosis
by Dr. Vardhan Joshi
Radiology plays an important part in diagnosing and characterizing the type of arthritis. Various
radiological modalities come handy for the purpose, however X-ray remains the most basic and most widely used modality.
X-rays can pass through the soft tissues of body, however are variably attenuated by calcium in bones giving rise to excellent pictures of bones, joints and articular surfaces. They also give an indirect idea of joint space and cartilage. In degenerative arthritis, there is joint space narrowing, subarticular sclerosis, erosions and osteophytes formation, while in rheumatoid arthritis there is initially joint space widening with periarticular osteopenia with soft tissues swelling. Slowly, there is joint space narrowing, articular erosion finally leading to ankylosis (bony fusion) and deformities. In psoriosis, there is abnormal bone formation, particularly along the sides of vertebrae with large osteophytes and occasionally bone sclerosis. In ankylosing spondylitis, spine has a “Bamboo” like appearance.
CT scan uses X-ray in a slightly different manner, to obtain thin sections of a body part and are used for evaluation of sacroilic joints, apophyseal joints.
MRI scan is based on imaging with strong magnetic field allowing us to visualize soft tissues like muscles, ligaments, cartilage and synovium like nerves before. It is particularly useful to visualize synovial hypertrophy in RA and to differentiate TB from arthritis. Atlantoaxial joints are also well evaluated with MRI. Sonography has nowdays been used for joint evaluation, particularly for joint fluid, status of capsule, ligaments and muscles.
Parameters studied in Rheumatic Disorders
by Dr. Anuradha Venugpaolan
Rheumatoid Factor How is it used?The test for rheumatoid factor (RF) is used to help diagnose rheumatoid arthritis (RA). About 65-70% of patients with this syndrome have high amounts of RF in their blood. However, in 30-35% of patients who are suffering from RA may not have RF in their blood. These are the seronegative group of patients in whom the disease may be less severe.
When is it ordered?The test for RF is ordered when you have signs of RA. Symptoms may include stiffness in your joints for a long time in the morning, swelling, nodules under your skin and evidence on X-rays of swollen joint capsules and loss of cartilage and bone if the disease has progressed. If you still have symptoms of RA but your first RF test is negative, the test may need to be repeated. The levels vary with the degree of symptoms and inflammation, and may be negative in periods of remission or inactive disease. The RF test also may be ordered to help diagnose other related disease e.g. Sjogren’s syndrome. Symptoms include extremely dry mouth and eyes, dry skin, and joint and muscle pain.
What does the test result mean?The latex test is reported in a titer with most labs considering > 1:40 as positive. The nephelometry test is usually reported in international units and the normal range is dependent on the specific laboratory usually < 20 IU.
The presence of significant values of RF indicates that you may have rheumatoid arthritis. Positive RF test results are found in the majority of cases of rheumatoid arthritis. Women more often have both of these diseases. About two to three times as many women as men have RA. The RF test may be positive in conditions other than RA such endocarditis, systemic lupus, erythematosus (lupus) syphilis, sarcoidosis, cancer, viral infection or disease of the liver, lung or kidney. You may also test positive if you have received skin or kidney grafts from a person who does not have your identical genetic profile. People with RA who are rheumatoid factor positive typically have a more aggressive disease.
A negative RF test result may not truly mean that you do not have RA. It may mean that it is too early in your disease progression to detect RF, or possibly you are in a remission phase. Numerically reported test results are interpreted according to the test’s reference range which may vary from population to population. In general, a value of more than 20 IU/ml is to be noted. A specific result within the reference (normal) range – for any test – does not ensure health
just as a result outside the reference range may not indicate disease.
The RF test has a high false positive rate,and the result must be interpreted along with the patient’s symptoms and history to make a diagnosis of RA or another condition. Interfering factors for the RF test generally include having many vaccinations or lipemia (a large amount of fats in the blood).
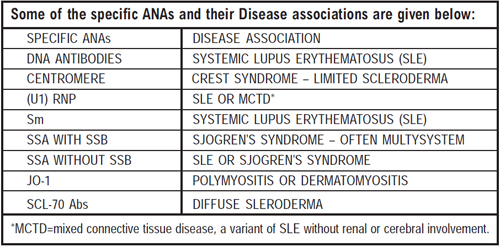
Antinuclear Antibody (ANA) How is it used?ANA, the standard abbreviation for Antinuclear Antibody, also referred to as ANF (antinulcear factor) is an expensive test but often misused by many doctors in interpretation. It requires consideration of the age of the patient, the titre of the antibody and most importantly: the exact specificity of the ANA.
When is it ordered?ANA is frequently ordered screening test, with a wide spectrum of clinical and lab features triggering its ordering – rashes, arthralgia and arthritis, pleurisy, alopecia and many others. Making sense of the result of the test is a frequent job for nearly every kind of medical practitioner.
What does the test result mean?ANA merely means that there is some kind of autoantibody present in a patient’s serum which is binding to some component of the nucleus of test cells in the laboratory. Each of these antibodies has a different
clinical significance. As an example, “positive ANA test” might be due to antibodies to DNA which are always significant and highly indicative of systemic lupus erythematous (SLE), a disease which is by no means rare in Caucasian females and is however relatively uncommon in Indians.
The titre of an ANA is not a perfect guide to the activity of an autommune disease. One patient with SSA antibodies giving an
ANA titre of 1:160 might have quite active SLE with photosensitivity, facial rash, mouth ulcers, and leucopenia, while another patient with SSA antibodies giving an ANA titre of 1:2560 might have only dry eyes from
primary autoimmune Sjogren’s syndrome.
In other words, antibodies titre needs to be weighed against the specific identification of the ANA, and even then it is an imperfect guide to disease activity. An exception to this is probably anti-DNA antibodies where titre is a relatively good guide to activity of SLE.
As a basic rule (with few exceptions) an ANA titre of less than 1:160 is usually not worth further analysis. Even when ANA has a high titre, e.g. 1:2560 it may still not indicate any significance disease.
AGE OF PATIENT : The incident of “positive’ ANA rises with age so it becomes common for 70-80 year olds to have low or even moderate titre ANA’s. An ANA of 1:640 will be common in a hospitalized 75 year old person with pneumonia. These “old age” ANAs seem to be mostly anti-histone antibodies and are not associated with autominnume disease. When the ANA is more closely analyzed the clinically significant ANAs i.e. DNA, RNP, SSA, SSB, or Scl 70 etc. are not more common in the elderly.
Anti Streptolysin ‘O’ How is it used?Anti-streptolysin O test,an internationally standardized test, is widely used in detection of group A streptococcal infections and their sequelae. Elevated or rising titres of ASO are seen in 80% or more of the case with
acute rheumatic fever.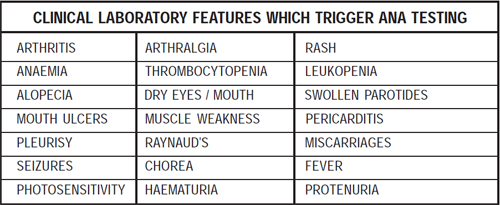
Some illnesses are caused by having had a Streptococcus bacteria infection sometimes in the past. These diseases may involve the heart, such as in rheumatic fever or scarlet fever. It may also include some kidney diseases.
The term “rheumatic” refers to synovial joints of the body (“rheum” refers to viscous fluid, such as synovial fluid), hence
“rheumatic fever” connotes an illness associated with abnormalities of synovial joints. When a common strain of bacteria
known as Streptococcus pyogenes, living in your throat and nose for months without causing any harm becomes active, they
produce an infection – sore throat initially and then certain disease conditions including the inflammation and swelling of
joints.
ASO shows up in the blood after a streptococcus infection. The presence of ASO does not tell which disease you have
now. It only tells there has been a streptococcus infection. The results of the test may be helpful to plan the treatment
for your illness. Several ASO tests may need to be done over a period of weeks.
The usefulness of streptococcal antibody data may be diminished if physicians or laboratory personnel are unable to knowledgeably interpret the levels of antistreptolysin O (ASO) or antideoyribounclease B (anti-DNase B) antibodies. Multiple variables, e.g. site of infection, time since the onset of infection, and age, have been shown to influence streptococcal antibody levels. In addition, an incomplete understanding of the kinetics of these immune responses may complicate
the interpretation. Clinical microbiology and immunology laboratories often use interpretative criteria suggested by
manufacturers of commercial antibody test kits. Because such “normal” levels may only reflect appropriate titers for adults (almost always lower than for children), correct interpretation of titers in children is important.
Acute and convalescent sera should be obtained and tested simultaneously to decide a rising ASO titer, but this is not
always feasible. Hence, a single specimen when available, requires to be compared with a pre-determined baseline value or an
upper limit of normal.
It there anything else I should know?
ASO titers can vary depending on the geographic locations, age group of the study population, and the climatic conditions. ASO titers more than 333 Todd units are generally considered elevated in children.
